I incorporate the best research, including my own studies into my treatment approach
The Specific Treatment for Problems of the Spine (STOPS) trial was completed in 2013 with the recruitment of 300 patients. It is the first randomised controlled trial showing moderate to large effects favouring the specific physiotherapy. The treatment evaluated was the same program that I developed and use with patients and in teaching practitioners on a daily basis. My research team from La Trobe University is currently working to publish this paper in a high quality journal. You can see some of the results in the graph below. It shows that specific physiotherapy is 50% more likely to result in a 50% improvement in daily activity capability compared to standard and guideline-based treatment. The evidence is clear; the treatment program I use and teach works!
From Adams (Clinical Biomechanics 2012)
What about the diagnosis
Current guidelines advise that diagnosing back pain is not possible (Koes et al 2010). Some even suggest that thinking about the injured structure when treating back pain may cause more harm than good (Dagenais et al 2010). However there is now reasonable evidence that using my clinical methods, injuries such as disc related pain can be identified and treated (Ford et al 2013). Part of this evidence is provided by an outstanding paper from Michael Adams that recommends practitioners think about the disc in the lumbar spine and how different treatments can actually increase the rate of healing. Some still doubt that healing in the disc is relevant to treating back pain. But look at the picture above; it is a cross section of an injured disc where a blood vessel has grown and is laying down scar tissue. A variety of physiotherapy methods can accelerate this healing process. These methods have been proven as successful in the STOPS trial.
Ford et al (Physical Therapy Reviews 2013)
Something for practitioners
There were 5 different treatment types in the STOPS trials. As we want to help as many people with back pain as possible, its important that these complex treatments were published for practitioners to access. Our papers (approximately 10,000 words each) have all been published in Physical Therapy Reviews and are available on our practitioner education website STOPS.physio.
This flow chart is an example of some of the decision making rules used in the STOPS trial to help practitioners negotiate difficult treatment scenarios. The example outlines clinical reasoning strategies when a person presents with back pain that has recently worsened.
More on diagnosis
This is another paper we have published on how to diagnose back pain; this time using an expert panel to establish diagnostic features. The paper, written by one of my PhD students Viktoria Wilde and myself, showed which features were more likely to be diagnostic of the zygaphophyseal (or facet) joint as the cause of a person's back pain. The results of this study converge with a range of other evidence to support the diagnostic features I use clinically and in the STOPS trial.
Treating back pain is complex
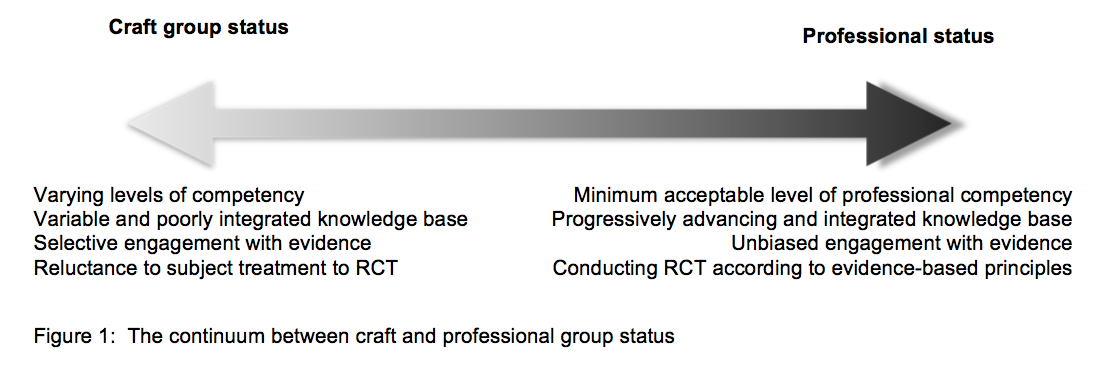
This figure is from a paper Andrew Hahne and I published on the complexity of treating back pain. In it, we urged practitioners of all disciplines to act professionally by using a progressive "building block" approach to acquiring evidence-based knowledge. We wrote this out of concern for some practitioners picking up on the latest "trends" in back pain research, rather than integrating new evidence with established current clinical practice. The aim of KALSI.com.au is to provide practitioners with a clear and structured approach to dealing with complex problems such as back pain.
References
1. Adams MA, Stefanakis M, Dolan P. Healing of a painful intervertebral disc should not be confused with reversing disc degeneration: implications for physical therapies for discogenic back pain. Clin Biomech 2010; 25(10): 961-71.
2. Koes BW, van Tulder M, Lin CW, Macedo LG, McAuley J, Maher C. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J 2010; 19(12): 2075-94.
3. Dagenais S, Tricco AC, Haldeman S. Synthesis of recommendations for the assessment and management of low back pain from recent clinical practice guidelines. The Spine Journal 2010; 10(6): 514-29.
Some of my papers
1. Ford J, Bennell K. Effectiveness of a physiotherapy functional restoration programme compared to patient-selected treatment on chronic compensable low back pain. Moving in on occupational injury. Oxford: Butterworth-Heinemann; 2000.
2. Hahne A, Ford J. Functional restoration for a chronic lumbar disk extrusion with associated radiculopathy. Physical Therapy 2006; 86(12): 1668-80.
3. Ford J, Story I, O’Sullivan P, McMeeken J. Classification systems for low back pain: a review of the methodology for development and validation. Physical Therapy Reviews 2007; 12: 33-42.
4. Heymans M, Ford J, McMeeken J, Chan A, de Vet H, van Mechelen W. Exploring the contribution of patient-reported and clinician based variables for the prediction of low back work status. Journal of Occupational Rehabilitation 2007; 17: 383–97.
5. Wilde V, Ford J, McMeeken J. Indicators of lumbar zygapophyseal joint pain: survey of an expert panel with the Delphi Technique. Physical Therapy 2007; 87(10): 1348–61.
6. Ford J, Story I, McMeeken J. The test retest reliability and concurrent validity of the Subjective Complaints Questionnaire for low back pain. Manual Therapy 2009; 14 283-91.
7. Hahne A, Ford J, Hinman R, et al. Outcomes and adverse events from physiotherapy functional restoration for lumbar disc herniation with associated radiculopathy. Disability and Rehabilitation 2010; Early Online: 1-11.
8. Hahne AJ, Ford JJ, McMeeken JM. Conservative management of lumbar disc herniation with associated radiculopathy: a systematic review. Spine 2010; 35(11): E488-E504.
9. Ford JJ, Surkitt LD, Hahne AJ. A classification and treatment protocol for low back disorders. Part 2: directional preference management for reducible discogenic pain. Phys Ther Rev 2011; 16(6): 423-37.
10. Ford JJ, Thompson SL, Hahne AJ. A classification and treatment protocol for low back disorders. Part 1: specific manual therapy. Phys Ther Rev 2011; 16(3): 168-77.
11. Hahne AJ, Ford JJ, Surkitt LD, et al. Specific treatment of problems of the spine (STOPS): design of a randomised controlled trial comparing specific physiotherapy versus advice for people with subacute low back disorders. BMC Musculoskelet Disord 2011; 12: 104.
12. Ford JJ, Hahne AJ, Chan AYP, Surkitt LD. A classification and treatment protocol for low back disorders. Part 3: functional restoration for intervertebral disc related disorders. Phys Ther Rev 2012; 17(1): 55-75.
13. Ford JJ, Richards MJ, Hahne AJ. A classification and treatment protocol for low back disorders. Part 4: functional restoration for low back disorders associated with multifactorial persistent pain. Phys Ther Rev 2012; 17(5): 322-34.
14. Richards MC, Ford JJ, Slater SL, et al. The effectiveness of physiotherapy functional restoration for post-acute low back pain: a systematic review. Manual Therapy 2012; 18(1): 4-25.
15. Slater SL, Ford JJ, Richards MC, Taylor NF, Surkitt LD, Hahne AJ. The effectiveness of sub-group specific manual therapy for low back pain: a systematic review. Manual Therapy 2012; 17(3): 201-12.
16. Surkitt LD, Ford JJ, Hahne AJ, Pizzari T, McMeeken JM. Efficacy of directional preference management for low back pain: a systematic review. Physical Therapy 2012; 92(5): 652-65.
17. Chan AY, Ford JJ, McMeeken JM, Wilde VE. Preliminary evidence for the features of non-reducible discogenic low back pain: survey of an international physiotherapy expert panel with the Delphi technique. Physiotherapy 2013; 99: 212-20.
18. Ford JJ, Hahne AJ. Pathoanatomy and classification of low back disorders. Manual Therapy 2013; 18(2): 165-8.
19. Ford JJ, Hahne AJ. Complexity in the physiotherapy management of low back disorders: clinical and research implications. Manual Therapy 2013; 18: 438–42.